Considerations of Remote Patient Monitoring in Heart Failure
Remote Patient Monitoring (RPM) use ranges from telephone based to complex technology based interventions
Approximately 10-20% of patients with exacerbations of heart failure are readmitted within 90 days.
Remote patient monitoring (RPM) potentially provides a cost effective solution to monitor patients between face to face visits.
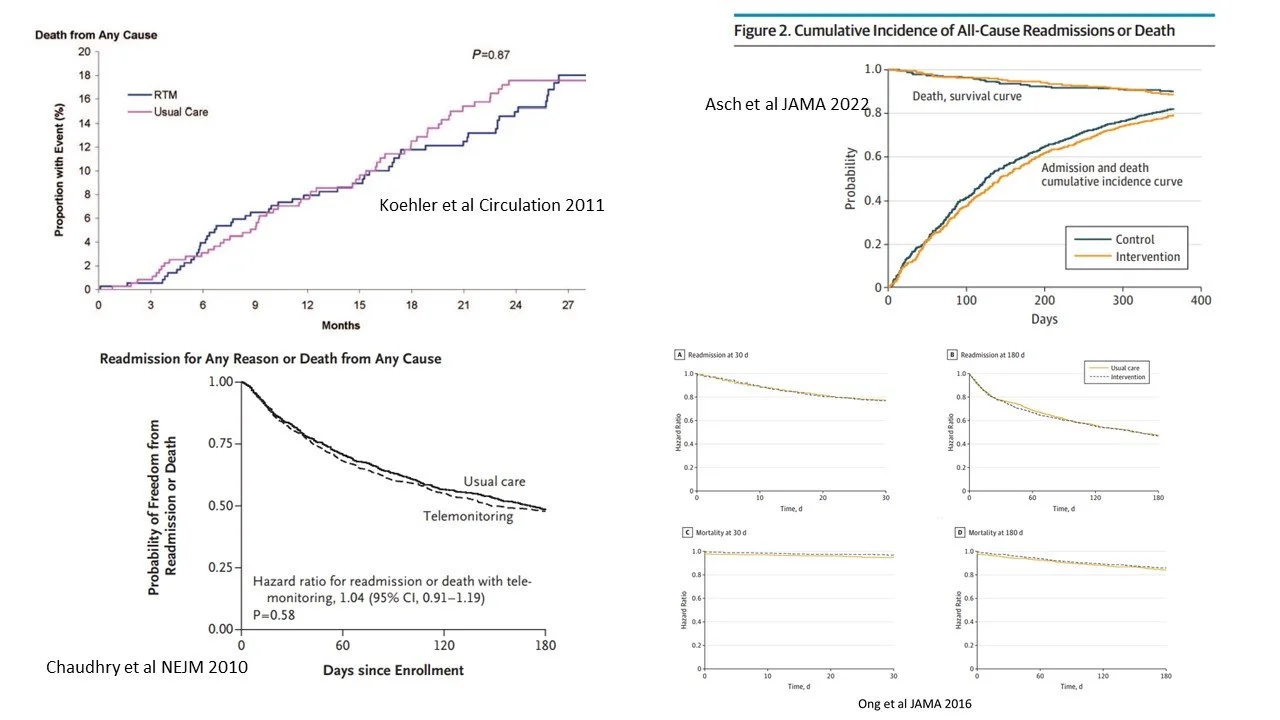
RPM in recently discharged patients with heart failure shown mixed and conflicting results in their ability to decrease hospital readmission and/or mortality rates.
Background
Heart Failure (HF) is a common condition affecting approximately 6 million patients in the United States.
HF is associated with high hospitalization and readmission rates, mortality and cost of care.
Patients are usually seen once their conditions decline to the point of severe symptomology, requiring acute care.
The hope of RPM is to engage the patient in self-monitoring to provide efficient care outside of face to face clinician visits.
The majority of cardiovascular RPM (CV-RPM) is considered non-invasive, with the transmission of data such as body weight, blood pressure, pulse oximetry, etc.
Review of the transmitted data can be active (regularly reviewed) or passive (only with a specific alert based on pre-determined threshold.
Less than 50% of published studies on RPM for all disease conditions have reported improvements in (Taylor et al, BMJ Open 2021;11:e040232):
Hospital admissions (49% of studies)
Length of stay (49% of studies)
ED presentations (41% of studies)
Review
Most Randomized Controlled Trials of CV-RPM are for heart failure patients.
Findings of these investigations have provided mixed results.
Studies vary in:
Patient groups studied
RPM devices used
Duration of RPM use
Intensity and timing of interactions.
Considerations For Success:
Integration of RPM data should directly be integrated into clinical practice for care of the patient.
Methods to re-enforce and improve patient engagement may improve outcomes
Newer technologies with greater invasiveness (i.e. implantable devices) may be provide better information.
CONCLUSIONS:
Studies claiming success with CV-RPM are based on small studies of patients with methodologic differences.
CV-RPM has not consistently demonstrated improvement in heart failure outcomes.
Further, thorough evaluations with broader integration of technology into clinical activities needs exploration.
Subscribe to the monthly newsletter here: http://eepurl.com/gFJKYD